TOP POSTS

While having a summer baby in Minnesota may sound easier than having a winter baby, there are still factors new parents must consider to help protect their babies from the heat.
Oral health refers to the overall state of your teeth, mouth, and gums, and it's a vital part of your overall health.
If you are pregnant with your second (or third or fourth) or are considering becoming pregnant, you may be wondering about the safety of continuing to breastfeed your baby or toddler throughout your pregnancy.
More than 23 million working parents in the US do not have an available caregiver in their family, according to a Brookings report
One of Dr. Amy’s passions is food introduction. It is a fundamental building block for a baby’s development, their immune system and has long-term health benefits.
Congrats! Your baby has arrived! This is a very exciting time for both parents.
The hottest days of summer can be tough on everyone but they can be exceptionally uncomfortable if you’re pregnant.
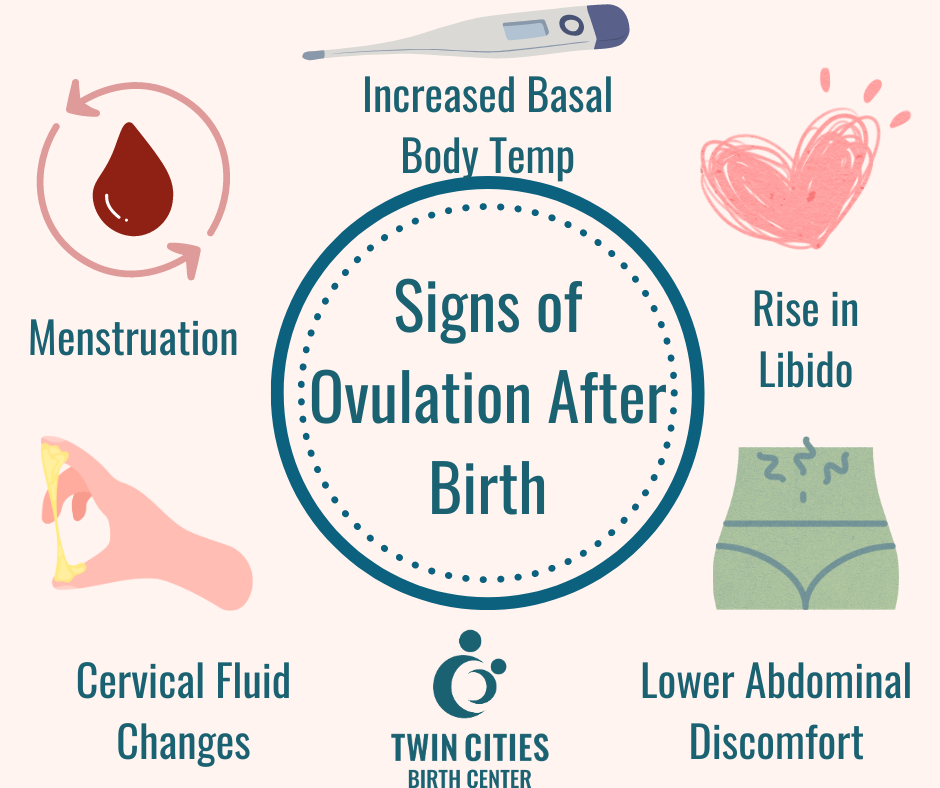
Everyone talks about what to expect during your pregnancy, but not enough discussion relates to what to expect after your pregnancy.
Whether it’s your first or your fifth pregnancy, the months following the birth of your child are completely unique times in your life.
Our thyroid function controls many different systems in our body. Shockingly, 1 in 8 women will develop thyroid disease.
Oral health refers to the overall state of your teeth, mouth, and gums, and it's a vital part of your overall health.
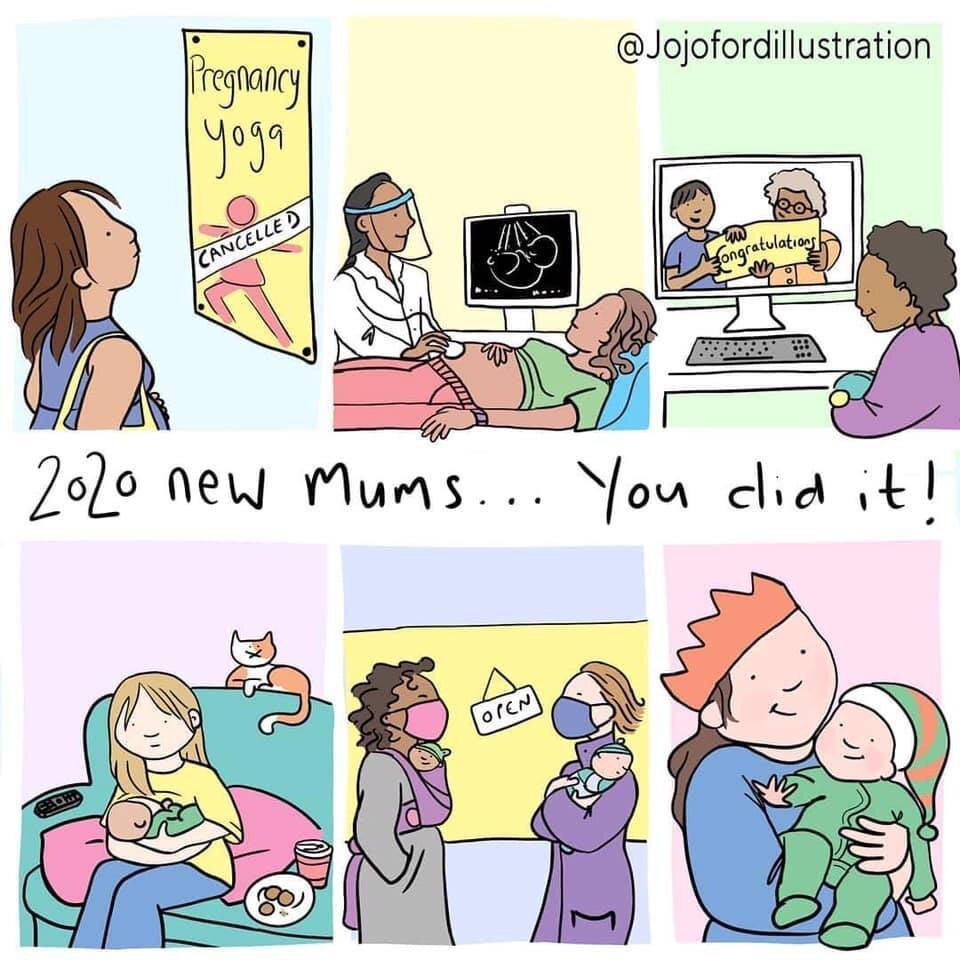
The pandemic has really made connecting with people complicated in so many ways. During the postpartum period, support is so vital.
Rhye’s story began in February 2020. When I randomly decided to take a pregnancy test, I fully expected it would be negative.
With water births becoming an increasingly popular natural birthing option, there are of course many misconceptions out there.
With pregnancy comes a lot of hormonal changes. These significant changes in hormones can cause cravings for certain food.
While we place a lot of emphasis on a woman's due date, the truth is these estimates of a baby's possible arrival are not very good indicators of when baby will actually be born. Believing this myth has the potential to set birthing families up for unwarranted pressure and stress and can lead to negative birth outcomes such as unnecessary testing, inductions, and c-sections. Learn more about estimated due dates here.

MEET OUR MIDWIVES
This is your birth, a completely personal event. At the moment of your birth and the precious moments following, our focus is to allow you the fullness of this time together with as little interference as possible.